Transcranial pulse stimulation (TPS)
Transcranial pulse stimulation (TPS) is a therapy option approved in Europe since 2018 for the treatment of mild and moderate Alzheimer’s dementia. Various regions of the brain are stimulated with shock waves to improve cognitive abilities.
The treatment is carried out over 6 days, spread over 2 weeks. Each therapy session lasts about 40 minutes. If there is a good response, sessions every 4 weeks are recommended as maintenance therapy. Refresher sessions with intensive treatment every few months or the combination with other stimulation methods, such as rTMS, are recommended.
How does TPS work?
Although shock waves are sound waves, unlike ultrasound with its periodic oscillations, shock waves are individual pulses with a high pressure amplitude. It is a mechanical stimulation, a kind of ‘reanimation’ of the brain cells.

Focussed shock waves are required for medical applications. These can be generated in various ways. For TPS with the Neurolith®, they are generated electromagnetically. The process is based on electromagnetic induction. As with loudspeakers, short acoustic pulses are generated by a special arrangement of coils and membranes and then emitted in a focussed manner with the help of a reflector.
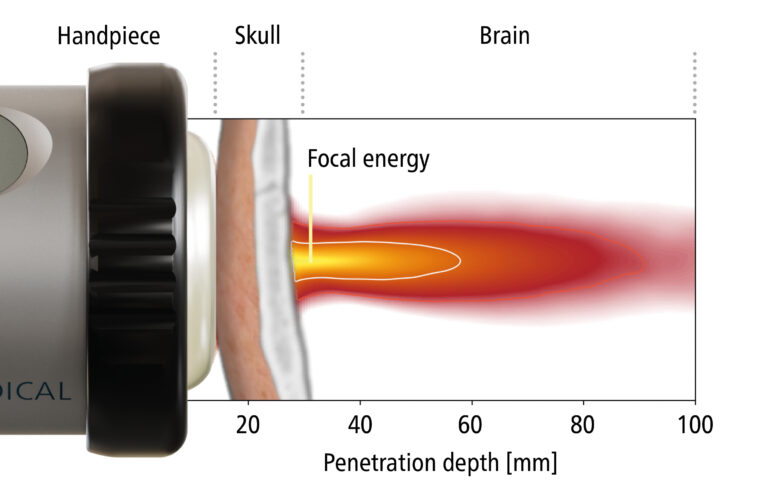
With TPS, shock waves (3 ms) are generated every 200 to 250 ms (4-5 Hz) to stimulate the brain tissue. With the Neurolith®, the brain regions can be stimulated up to 8 cm deep. With an applied energy of 0.2 mJ/mm2, the risk of tissue heating and thus tissue damage is prevented. An infrared camera system allows real-time tracking of the handpiece position (transducer), which is automatically visualised by using personal MRI data. In the very commonly used stimulation protocol, the frontal, temporal and parietal cortex are stimulated in addition to the precuneus to treat all important networks associated with memory.
TPS explained - Video
Überschrift

Mechanosensitive ion channels play a key role in the biological effect. As they lead to an increase in cell permeability, there is a change in the concentration of neurotransmitters (increase in serotonin and dopamine, decrease in GABA) and neurotrophic growth factors (increase in VEGF, BDNF and GDNF).
Mechanosensitive Ion Channels
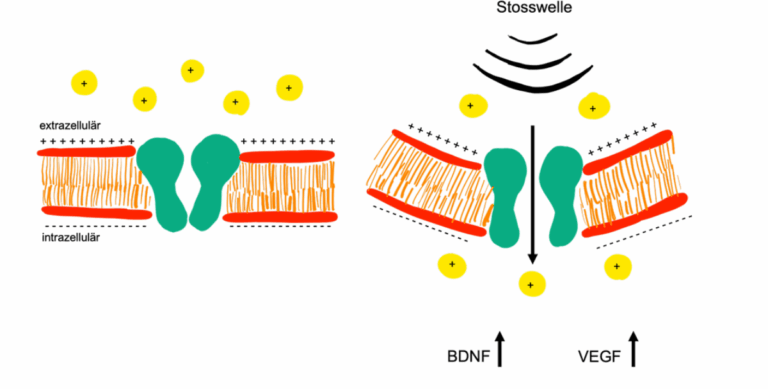
The stimulation of the vascular growth factor VEGF (Vascular Endothelial Growth Factor) leads to the formation of new blood vessels and thus to an improvement in blood flow to the brain.
The concentration of the growth factor BDNF (Brain-Derived Neurotrophic Factor) is also increased by the shock waves. This plays a major role in the development and maturation, but also in the regeneration of nerve cells and in neuroneogenesis (the formation of new nerve cells) and therefore neuroplasticity in the brain.
Since when has TPS been used?
The term ‘sound shock waves’ is used in orthopaedics (treatment of tendinopathies) and urology (treatment of erectile dysfunction) to describe sound wave pulses that do not destroy the tissue but stimulate it and promote regeneration. In recent years, transcranial pulse stimulation (TPS) has been developed with the aim of alleviating the symptoms of Alzheimer’s dementia by stimulating the brain tissue.
What are the results of treatment with TPS?
The research results available so far are very promising. However, innovation always needs time to be recognised by all medical professionals.
One study showed that an improvement in cognitive function was possible after just 6 treatment sessions, which remained stable for 3 months. In a further study, an antidepressant effect of TPS was also demonstrated in patients with Alzheimer’s dementia.
It can be assumed that all procedures that improve neuroplasticity promote the positive result of the shock wave (e.g. rTMS, ECT, esketamine, psychotherapy, certain medications).
What side effects can occur with TPS?
Side effects that can occur: So far, only harmless side effects have been described when used correctly (observing the indication and contraindication), as the sound pulses are dosed in such a way that they cannot lead to tissue injury.
When can TPS not be used?
The treatment cannot be carried out in these situations: Coagulation disorder, cortisone treatment in the last 6 weeks, implanted intracranial electrodes, cochlear implant, previous brain surgery, ventriculo-peritoneal shunt, brain tumour, certain vascular diseases (severe leukoencephalopathy, amyloid angiopathy).
Are the costs covered by health insurance?
The costs of Transcranial Pulse Stimulation (TPS) treatments are not covered by basic health insurance. However, you can clarify whether your supplementary insurance (e.g. for innovative treatments) will cover part of the costs.
Trending:
Does TPS have an effect on stem cells?
1. In vitro findings (cell culture)
In cell culture models, it has been shown that TPS stimulates the proliferation and differentiation of neural stem cells. The underlying effect is based on mechanical micropulses that activate cellular signaling pathways through mechanotransduction (Beisteiner et al., 2019). Neurotrophic factors such as BDNF, VEGF and NO were increasingly released, resulting in improved cell activity and migration (Matt et al., 2022).
Beisteiner et al (2019): Transcranial Pulse Stimulation with Ultrasound in Alzheimer’s Disease – A New Navigated Brain Therapy. Advanced Science, 6(3), 1801852.
Matt et al. (2022): Transcranial Pulse Stimulation induces neurogenesis and neurotrophic signaling in human neural stem cells. Cellular and Molecular Neurobiology, 42, 3813-3825.
2. In vivo and clinical data
In a prospective pilot study with Alzheimer’s patients (n = 35), TPS showed significant improvements in cognitive performance (CERAD score), accompanied by sustained activation of neuroplastic processes (Beisteiner et al., 2020). In addition, imaging techniques indicated functional neuroplasticity and network changes in the brain.
Further studies have demonstrated indirect activation of neural stem cells via TPS-initiated microvascular processes and inflammatory modulation (Plazak et al., 2023).
Beisteiner et al (2020): Functional MRI-Guided, Navigated Transcranial Pulse Stimulation in Alzheimer’s Disease. Brain Stimulation, 13(6), 1794-1801.
Plazak et al. (2023): Long-term effects of transcranial pulse stimulation (TPS) on brain function and structure in Alzheimer’s disease. Journal of Neurology, 270, 4048-4057.
References
Beisteiner R, Lozano A. Treating the brain at the speed of sound. Brain Stimulat. August 2020;13(4):1087–8.
Beisteiner R, Matt E, Fan C, Baldysiak H, Schönfeld M, Philippi Novak T, u. a. Focal Brain Therapy: Transcranial Pulse Stimulation with Ultrasound in Alzheimer’s Disease—A New Navigated Focal Brain Therapy. Adv Sci. Februar 2020;7(3):2070017.
Matt E, Dörl G, Beisteiner R. Transcranial pulse stimulation (TPS) improves depression in AD patients on state-of-the-art treatment. Alzheimers Dement N Y N. 2022;8(1):e12245.
Jeong H, Im JJ, Park JS, Na SH, Lee W, Yoo SS, u. a. A pilot clinical study of low-intensity transcranial focused ultrasound in Alzheimer’s disease. Ultrason Seoul Korea. Oktober 2021;40(4):512–9.
d’Agostino MC, Craig K, Tibalt E, Respizzi S. Shock wave as biological therapeutic tool: From mechanical stimulation to recovery and healing, through mechanotransduction. Int J Surg Lond Engl. Dezember 2015;24(Pt B):147–53.
López-Marín LM, Rivera AL, Fernández F, Loske AM. Shock wave-induced permeabilization of mammalian cells. Phys Life Rev. November 2018;26–27:1–38.
Yahata K, Kanno H, Ozawa H, Yamaya S, Tateda S, Ito K, u. a. Low-energy extracorporeal shock wave therapy for promotion of vascular endothelial growth factor expression and angiogenesis and improvement of locomotor and sensory functions after spinal cord injury. J Neurosurg Spine. Dezember 2016;25(6):745–55.
Hatanaka K, Ito K, Shindo T, Kagaya Y, Ogata T, Eguchi K, u. a. Molecular mechanisms of the angiogenic effects of low-energy shock wave therapy: roles of mechanotransduction. Am J Physiol Cell Physiol. 1. September 2016;311(3):C378-385.
Mariotto S, Cavalieri E, Amelio E, Ciampa AR, de Prati AC, Marlinghaus E, u. a. Extracorporeal shock waves: from lithotripsy to anti-inflammatory action by NO production. Nitric Oxide Biol Chem. März 2005;12(2):89–96.
Ledo A, Lourenço CF, Cadenas E, Barbosa RM, Laranjinha J. The bioactivity of neuronal-derived nitric oxide in aging and neurodegeneration: Switching signaling to degeneration. Free Radic Biol Med. Januar 2021;162:500–13.
Wang B, Ning H, Reed-Maldonado AB, Zhou J, Ruan Y, Zhou T, u. a. Low-Intensity Extracorporeal Shock Wave Therapy Enhances Brain-Derived Neurotrophic Factor Expression through PERK/ATF4 Signaling Pathway. Int J Mol Sci. 16. Februar 2017;18(2):E433.
Matt E, Kaindl L, Tenk S, Egger A, Kolarova T, Karahasanović N, u. a. First evidence of long-term effects of transcranial pulse stimulation (TPS) on the human brain. J Transl Med. 15. Januar 2022;20(1):26.
Popescu T, Pernet C, Beisteiner R. Transcranial ultrasound pulse stimulation reduces cortical atrophy in Alzheimer’s patients: A follow‐up study. Alzheimers Dement Transl Res Clin Interv [Internet]. Januar 2021 [zitiert 12. Februar 2022];7(1). Verfügbar unter: https://onlinelibrary.wiley.com/doi/10.1002/trc2.12121
